July 25, 2018
Webinar Highlights: Are You Optimizing the Performance of Your Emergency Department?

 When it comes to improving the performance of your department, engagement should be your top priority. Colleagues and hospital leaders need to be aligned and engaged to truly provide the best care and increase performance of your department. You must also have buy-in from key stakeholders to drive performance. I recently hosted a webinar along with Dan Smith, MD, FACEP, Senior Coach and Executive Medical Director of Studer Group, to discuss the importance of engagement and how it relates to department optimization.
When it comes to improving the performance of your department, engagement should be your top priority. Colleagues and hospital leaders need to be aligned and engaged to truly provide the best care and increase performance of your department. You must also have buy-in from key stakeholders to drive performance. I recently hosted a webinar along with Dan Smith, MD, FACEP, Senior Coach and Executive Medical Director of Studer Group, to discuss the importance of engagement and how it relates to department optimization.
Why Have an Engaged Team?
To optimize the emergency department, you must start with an engaged team. It is the culmination of commitment, contribution, and fulfillment. When your workforce is engaged, it results in:
- Improved loyalty and patient experience
- Increased market share
- Decreased litigation
- Improved provider recruitment and retention
- Improved safety and quality outcomes
- Improved measures on national metrics
As Dan says in his book titled Advance Your Emergency Department: Leading in a New Era, “Consistent collaboration is the ‘secret sauce’ that pulls the whole model together and differentiates a truly great ED from a good one.” According to Studer Group’s Straight A Leadership assessment of over 37,000 leader responses in 577 hospitals, higher workforce engagement directly results in high patient engagement. 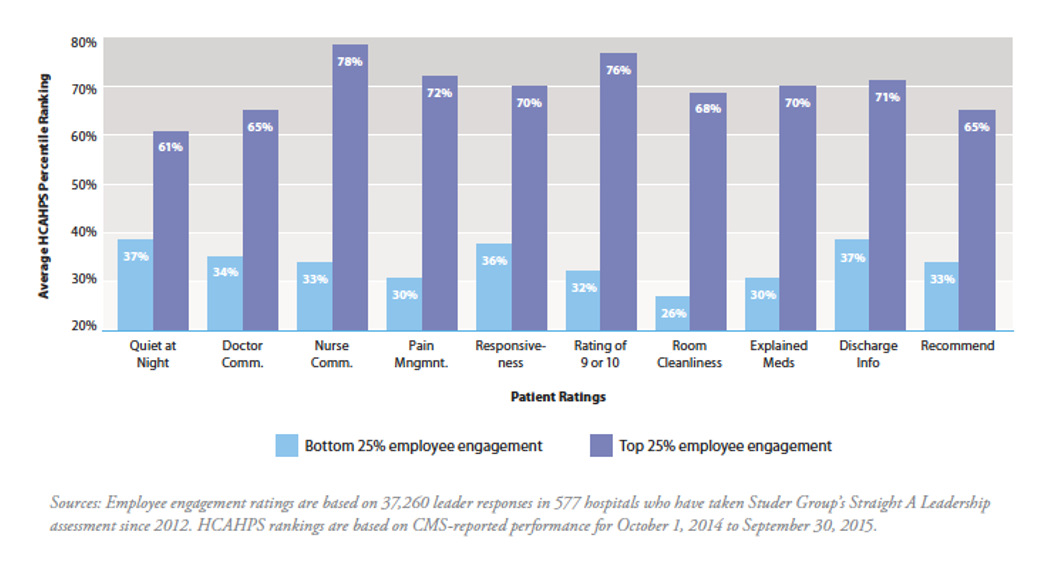
How to Improve Team Engagement
There’s a corelation between better patient engagement and engaged physicians. So, how do you identify which colleagues are engaged? Try using the acronym I CARE.
- Input and skills
- Care quality
- Appreciation
- Responsiveness and feedback
- Efficiency
There are numerous strategies to help promote engagement but one of the most consistent, high impact tactics for leaders is leader rounding on colleagues. By having a reoccurring interaction with your direct reporting clinicians, you can better understand them and what they need. When you are rounding, you should align questions to fit the desired outcomes of the organization and to build relationships with your colleagues. Ask questions around the following topics:
- Concern and care
- What is working well?
- People to recognize
- Systems to improve
- Tools and equipment
- Follow-up
Finally, be sure to recognize colleagues for their good work. While financial recognition can be one approach, don’t overlook the power of handwritten notes, as well as highlighting colleagues in newsletters or meetings. A small gesture can have just as big of an impact.
The Impact of Operational Flow Efficiency
Having team buy-in leads to improving operational flow efficiency of your department. But why does improving efficiency matter? In emergency medicine, we measure all of our operational throughput metrics down to the minutes and sometimes down to the seconds. Physicians should challenge themselves to think about minutes and seconds not only as a measure of time, but also as a quality metric. On average, the shorter the time to provider is, the less likely it is that you’ll be named in a claim. Many times, in the first few minutes, a provider can identify what is going on and communicate solutions to help the patient. Yes, their wait time is shorter, but more importantly, you provide care to the patient more quickly. If you’re able to improve the flow of the ED, then you can get in front of your patients quicker. Although timing is important to providing high-quality care, sometimes you aren’t able to provide care as quickly as you might prefer. 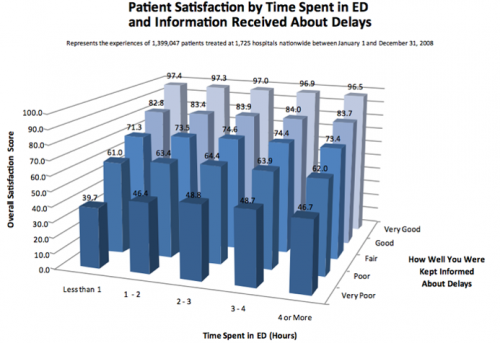 By communicating with a patient about what to expect during their visit regarding expected delays, you can improve patient satisfaction. Most patients understand that the ED is busy, so keeping them informed helps them know what to expect. In a Press-Ganey survey, it was found that if a patient is kept informed about delays, they left feeling more satisfied, regardless of the actual time spent in the hospital. Data can impact where an individual chooses to seek care. The data that we collect is publicly reported, and patients are using that data in their decision making process. To provide high-quality care, you must be able to improve efficiency to reduce wait times.
By communicating with a patient about what to expect during their visit regarding expected delays, you can improve patient satisfaction. Most patients understand that the ED is busy, so keeping them informed helps them know what to expect. In a Press-Ganey survey, it was found that if a patient is kept informed about delays, they left feeling more satisfied, regardless of the actual time spent in the hospital. Data can impact where an individual chooses to seek care. The data that we collect is publicly reported, and patients are using that data in their decision making process. To provide high-quality care, you must be able to improve efficiency to reduce wait times.
How to Improve Emergency Department Flow Efficiency
As you can see, improving flow efficiency is vital to the success of an ED. In order to improve flow efficiency, you must identify waste, which can include waiting, neglect, transportation, inventory, motion, and excess. Identify areas you can improve to help reduce waste and improve efficiency. Optimizing staffing is critical to improving flow and driving safety, quality, and service. Clinicians can be think-tanks and communicators, adding value to patient care, medical decision-making, and building relationships with patients. When putting together a team, identify individuals that can promote effectiveness, flow efficiency, resource stewardship, professionalism, and team wellness. To further improve the efficiency of your ED you may want to re-evaluate the design. The process of care and operational flow should dictate physical design and room/care space characteristics. First, ask yourself, “Is the current structure constraining or supporting flow?” Then, think of ways to make your physical design patient-centered, provider-friendly, and functional. Remember, more beds isn’t always the answer.
Why Patient Engagement Matters
To improve the metrics of an ED, you must improve patient experience and provide high-quality patient interactions. The old model of volume-based care has been replaced with value-based care. Now, more than ever, you can easily access reviews of practicing physicians on many different social media sites. If you don’t engage with them, it will quickly be known. The healthcare landscape has shifted. The old model of “usually” has shifted to “always,” and providing “good” care now means “excellent.” The focus is on the outcomes you are delivering and the patient experience. The success or failure to deliver on these fronts has a direct correlation to hospital and provider financial performance with value-based purchasing.
How to Improve the Patient Experience of Care
Patients now expect to receive the whole package when they visit the emergency department. They want timeliness, a team approach, effective care, clear communication, and they want to feel like their provider cares. Improving the flow of the ED is just one aspect of the package. Physicians must also adopt new habits when communicating with their patients. Some common doctor communication elements that help improve patient experience includes:
- Respect
- Listening
- Explaining
- Instructing
- Informing of delay
In addition to different communication elements, it is vital that providers display empathy to those they serve. Some attributes of empathetic providers include:
- Warm tone
- Proximity
- Eye contact
- Admiration
- Acknowledgment
- Therapeutic touch
- Listening keywords
Using these different skills can ensure that you provide an excellent patient experience, feel more fulfilled as a physician, reduce risks, and improve value-based outcomes. When you have an engaged team, you can work together to better operational flow efficiency and improve the overall patient experience.
View the webinar
To watch the full webinar on improving the performance of your emergency department, click here.
