September 19, 2018
Sepsis Care Revisited

During September, hospitals across the U.S. are raising awareness for Sepsis Awareness Month. This seems to be a perfect opportunity to revisit our approach to sepsis care. Numerous hospitals around the country are actively working on improving the delivery of care for patients with sepsis. Many of these hospitals are struggling and will likely use Sepsis Awareness Month as an opportunity to shine a bright light on their sepsis initiatives and perhaps get a boost of momentum in the right direction. For over a decade, clinicians have focused on the use of bundles and guidelines to improve care at the bedside. Furthermore, regulations from CMS and state-based agencies have created a heightened focus on sepsis from hospital administrators. Sepsis has become a constant topic of discussion at all levels – clinical, academic, administrative, policy, and research. As sepsis receives increased attention, it seems that many efforts and initiatives related to improving care have taken lives of their own and perhaps have moved in directions that impede a clear visualization of what we are truly trying to achieve. I would like to take the opportunity to revisit sepsis care and briefly touch on the why, the how, and the what as they relate to our performance improvement efforts.
Why?
Sepsis is a complex syndrome. Improving care for sepsis requires a team effort and high levels of engagement from multiple disciplines within the hospital. Unfortunately, too often, healthcare providers are dragged into sepsis committees and told about new things they need to do to improve sepsis care without any mention of why these efforts are important. Let me start by making it clear that regulatory requirements are not a great why or motivator to that effect for healthcare providers. Sepsis is the leading cause of mortality, morbidity, and cost of care in hospitalized patients in the United States. That is the real why. Our goal is to improve outcomes for our patients. This is definitely a why the vast majority of health care providers can rally around. Making a difference for others is a huge motivator. Understanding the scope of the problem with sepsis and being clear on the opportunity to move the needle is even more powerful. As we move forward with any effort to improve care, we should always keep present the ultimate goal and why we started the effort in the first place. Reducing mortality, decreasing morbidity – those are the outcomes we should be tracking on a regular basis. Process metrics are only a means to making a real difference in patient outcomes. Let us not lose sight of what really matters at the end. We meet and work together on better ways of delivering care in sepsis because we want to improve outcomes for our patients. That is the why.
How?
How should we approach this problem? The first word that comes to mind is “together.” Sepsis is not a physician problem, and it is not confined to the intensive care unit. Sepsis affects patients in different areas of the hospital, and delivering care to these complex patients requires the full engagement of a platitude of health care disciplines. Sound Physicians, as the expert in providing the highest value for patients during their acute care episode, will lead the way. Making a dent in sepsis outcomes requires reliable processes of care that connect the emergency department with the intensive care unit and with the medical floors. Furthermore, it requires a deliberate design that assures all disciplines (nursing, physicians, advanced practice providers, pharmacists, etc.) are reliably at their maximal point of contribution to assure patients receive the right treatment at the right time, every single time. Working in silos will not get us there. We must understand that improving sepsis requires a committed and engaged team.
What?
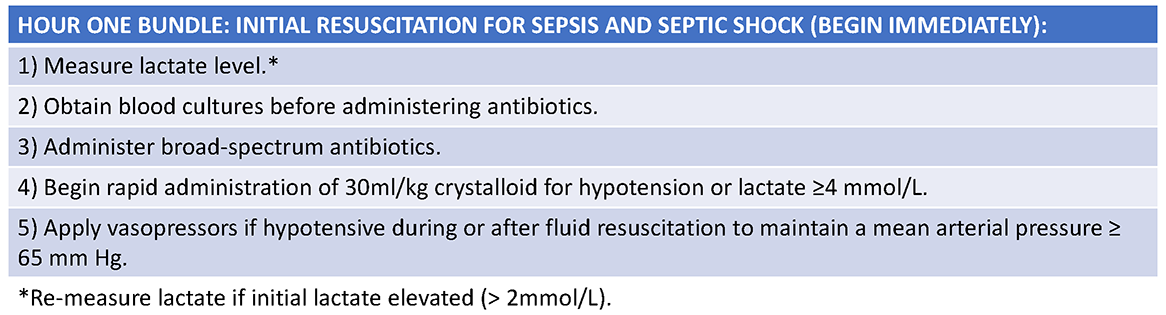
What we should do for sepsis is simple, but we sure insist on making it more and more complicated. Simple does not mean easy. In order to improve outcomes in patients with sepsis, we must work together as a team to 1) identify patients with infection and acute organ damage as soon as possible, and 2) in these patients, implement time-sensitive interventions as quickly as possible. Identification requires education efforts throughout the hospital. Sepsis is still a syndrome, and the use of terms such as sepsis, severe sepsis, and septic shock still create confusion amongst health care providers and are a source of great debate amongst experts. Without diving into the world of sepsis definitions, let’s focus on patients with a new infection and acute organ dysfunction. This is the key patient population that we are trying to identify. If we work on making sure healthcare providers think of these two items (infection and organ dysfunction), we will surely identify patients with sepsis earlier. Finally, the reason early identification is important is the ability to intervene with time-sensitive treatments, such as appropriate antibiotics and hemodynamic support (intravenous fluids and vasopressors when fluids are not enough). These interventions need to be initiated as soon as possible, preferably within the first hour of identifying the patient with sepsis or septic shock (Table 1).
Table 1
 Final Thoughts
Final Thoughts
Sepsis is a leading problem in our current healthcare environment, causing an enormous impact on hospitalized patients and healthcare costs. We must work together with the sole objective of improving patient outcomes. Improved outcomes are predicated on our ability to consistently identify sepsis patients early and implement time-sensitive, lifesaving interventions (antibiotics and hemodynamic support). During Sepsis Awareness Month let’s not lose sight of the why, the how and the what.
