June 18, 2020
Determining Correct Admission Status for COVID-19 Patients

Deciding on the correct admission status for COVID-19 patients is the first step toward proper hospital and provider reimbursement. Because of the unpredictable course of COVID-19 infection, it is especially challenging for physicians to choose an appropriate initial admission status, which is further complicated by COVID-19 testing issues.
Current diagnostic tests (RT-PCR), authorized by the FDA under emergency use authorization, have about 71% to 75% sensitivity, which means that up to 30% of symptomatic COVID-19 patients may have a false-negative test. Thorough clinical assessment and documentation, including risk factors, is paramount. As well, it’s vital to remain current on rapidly changing clinical criteria for COVID-19 admissions and to understand the factors that can prevent COVID-19 denials.
Your decision whether to admit the patient to the hospital depends on three factors.
- Vital signs on admission: The key is the presence of hypoxia, defined as pulse ox less than 94%.
- Patient risk factors: Age, comorbidities, immune deficiency, altered mental status, or evidence of lower respiratory tract infection.
- Risk factors for progression to severe disease: Elevated D-dimer, CPK, CRP, LDH, transaminases, troponin or lactate; low absolute lymphocyte count; extensive bilateral and/or worsening pulmonary infiltrates, and failed 1-minute walk test.
Using these factors, you can identify patients who can be discharged from the ED, admitted to hospital, including the intensive care unit, or placed in observation.
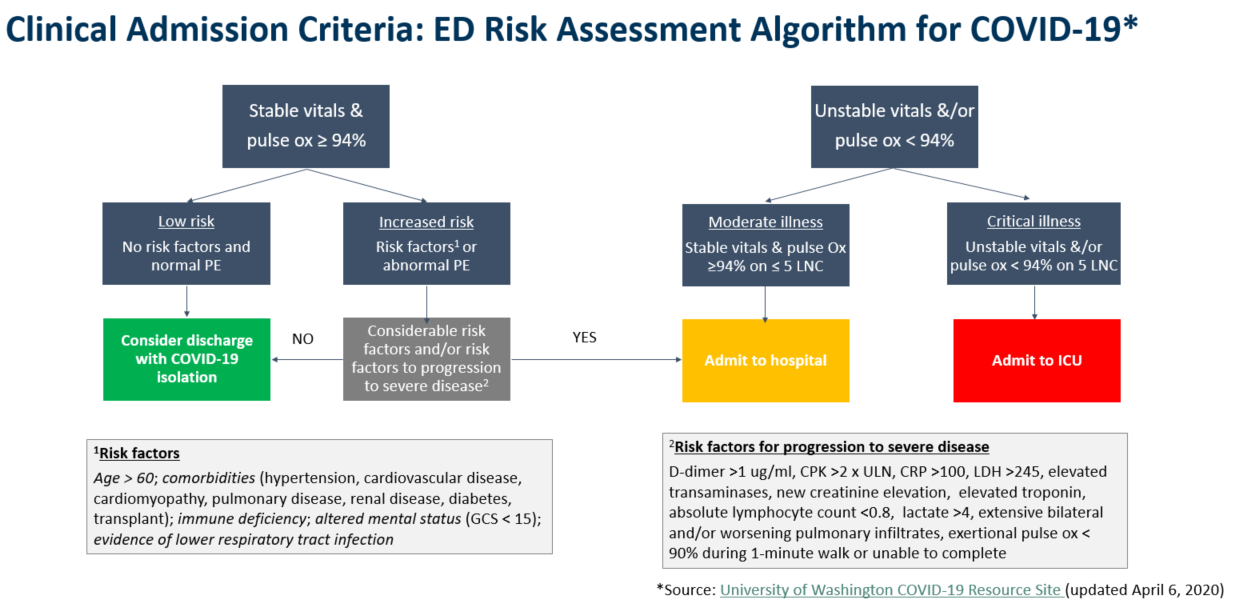
Generally, patients can be discharged from the ED if they are clinically stable, do not have any risk factors, are not at risk for progression to severe disease, and can be safely isolated at a low level of care. Patients who have oxygenation less than 94% on room air require hospitalization. And, if they have hemodynamic instability or need more than five liters of oxygen to maintain oxygenation above 94%, they are at high risk for rapid deterioration and are candidates for admission to ICU.
Patients in the gray zone are clinically stable right now, but they have risk factors, including for progression to severe disease. These patients are appropriate for observation. In all cases, documentation must be specific and clear about why their status aligns with their level of care.
Other tools that help to risk-stratify include the MuLBSTA Score for Viral Pneumonia Mortality, which looks at six different criteria to predict a 90-day mortality rate for those patients. MCG’s Acute Viral Illness Guidelines are also available to help determine an appropriate status, particularly for commercial patients, and can be downloaded free of charge.
It is worth noting that, in otherwise clinically stable patients without high risk for clinical deterioration, the need for isolation that cannot be performed outside of a hospital setting will not -on their own- justify observation or inpatient stay.
The 1st wave of denials for COVID-19 admissions may be just the tip of the iceberg, and we know more are coming. Now is the time to reinforce clear and specific documentation as the key to preventing denials. Seemingly small details, such as oxygenation on room air, presenting physical findings (for example accessory muscle use, or suprasternal, intercostal or subcostal retractions), patient risk factors and risk factors for progression to severe disease, including 1-minute walk test, can prevent the denial of an entire hospital stay.
Learn more in this complementary 30-minute webinar.
Dr. Farah presented on this topic in the Sound Advisory Services webinar, COVID-19 Admissions: Getting Status Right & Preventing Denials. Click here to watch the webinar.
Sound Physician Advisory Services has a weekly newsletter, The Physician Advisor, where experts have curated relevant news articles, resources, and tools, along with breaking news on the pandemic into one newsletter. Click here to subscribe.
Sources:
