November 16, 2017
Bad Air
“Mala Aria,” or malaria as we call it today, is ancient Italian for “bad air.” Given the prevailing theory of disease transmission all the way through Victorian times, Malaria was aptly named. That theory, miasma, suggested diseases like cholera or even the plague spread via noxious air. Diseases just floating along infecting those unfortunate enough to come into contact with its cloud. A vile pollution. While that may seem absurd today, it’s no more illogical than the notion that an army of microorganisms, undetectable to the eye, was invading convalescing bodies and wounds. Causing the infections and concomitant suppuration that so often claimed life early in those days. You can imagine, when the heavy doors to the Glasgow Royal Infirmary burst open one morning with a boy who suffered a compound fracture to his leg (a shard of the bone was poking out of the skin) things looked dire. It was 1860’s Scotland. Infection and sepsis killed most it touched. And a compound fracture is an open door for disease to walk through.
Taking a different approach
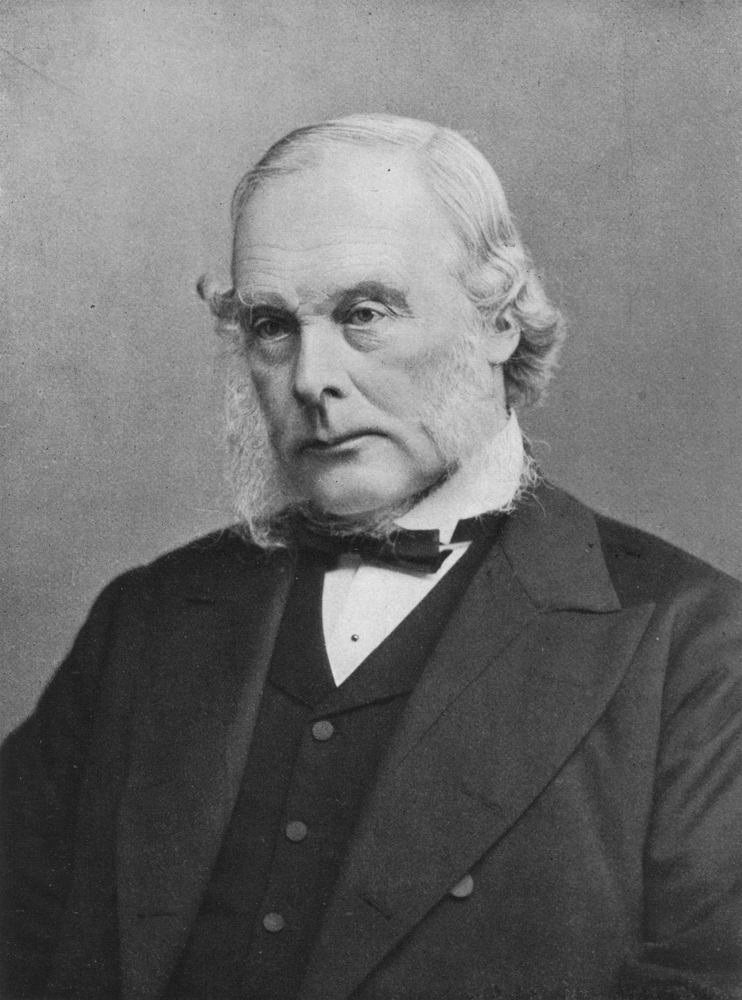
On that particular day, the surgeon greeting the young boy at the infirmary was Dr. Joseph Lister. Trained in London, apprenticed in Edinburgh, and now a professor of surgery in Glasgow, Dr. Lister had seen his fair share of the consequences of this particular fracture. He knew the sequelae was going to cause infection of the bone or surrounding tissue, but he also knew the standard treatment of the day — amputation — conferred an unacceptably high mortality as well; likely due to infection from the surgery itself. In addition, this was a young man in a time when disability benefits were non-existent or workplace accommodations. Amputation for this boy would result, at best, in a man unable to work, lead a successful life, or contribute to society. The surgeon, Dr. Lister, decided to take a different approach and not operate. Instead, based on his own research that built upon the work of French chemist Louis Pasteur, Dr. Lister systematically and repeatedly applied his own concoction of carbolic acid to the wound and set the fracture. He theorized that if the disease was in the air, and that disease was, in fact, a germ, he would make the wound such an inhospitable environment for the germ it would never invade. Again and again, day after day, Dr. Lister applied carbolic acid to the wound. With this new method surgical mortality fell from 45 to 15 percent in his Male Accident Ward.
Creating long lasting change in medicine
In 1867, Dr. Lister published his findings on anti-sepsis in a series of cases. He methodically cataloged his work for others to replicate. He and his germ theory were not well received. The surgeons of the day did not react kindly to the notion that their lack of hygiene resulted in direct harm to their patients. Approximately 20 years earlier in Vienna, Dr. Ignaz Semmelweis stumbled upon the finding that only washing one’s hands before delivering a baby reduced the likelihood of puerperal fever. And therefore dropped the associated mortality rate by more than half. Dr. Semmelweis was so fervent about his discovery, and so poorly received; he was eventually committed to an asylum where he, unfortunately, died of sepsis at the age of 47. Unlike Dr. Semmelweis, Dr. Lister was able to enjoy recognition for his findings in germ theory and his contributions to modern surgery in his later life. Yet, he had to overcome many who were skeptical. Across the pond at Massachusetts General (Harvard Medical School), they not only rejected Dr. Lister’s idea of anti-sepsis they took the additional step of banning the practice at the institution. Dr. Lister never wavered. He knew the data because he collected and cataloged it. He knew his rates of infection, sepsis, and mortality was notably lower than his counterparts. He knew that his patients did better. Physicians are trained to be skeptical of change, leery of the new. And for very good reason. But we should also remember the history of medicine’s lesson: that today’s standard of care will likely not be the standard of care years from now. That the way it’s done will not be the way it will always be. We should remember to not only be skeptical of the new, but also the status quo.
