May 7, 2020
Sound Physicians combats COVID surge with telemedicine and innovative care design
Amid the spreading coronavirus pandemic, the state of Maryland was grappling with how to manage a surge in COVID-19 patients, which prompted the state’s governor to issue an executive order to increase the hospital capacity by 6,000 beds. To help fill the potential bed shortage, Maryland identified three sites, including the University of Maryland Laurel Medical Center (UM Laurel), which had previously closed due to low patient volumes.
At the governor’s direction, in partnership with the Maryland Department of Health (MDH), the University of Maryland Medical System (UMMS) and UM Capital Region Health, Sound Physicians was chosen to develop and deploy a full-service care plan to help meet the pending patient demand as Maryland was about to hit a peak in COVID-19 cases.
“During this critical time of need, we turned to our trusted partners, Sound Physicians,” said Trudy Hall, Executive Site Lead, VP of Clinical Operations, UM Laurel COVID Hospital. “It made sense to have an integrated approach to focus on quality of care as we journey thru this pandemic and Sound was instrumental in the planning and operating process, for a successful go-live at UM Laurel in two weeks.”

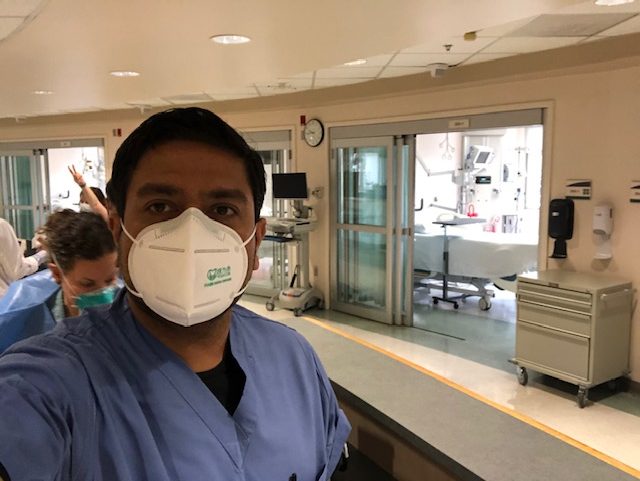
“Before we could propose a surge plan with confidence, we researched feasibility to determine if we could meet the staffing challenges in an already taxed healthcare circumstance that included PPE shortages and shrinking budgets,” said Dr. Minesh Patel, Regional Medical Director. “Fortunately, we were able to pull all of the right levers by utilizing telemedicine and temporary staffing, and our longstanding, successful partnership with UM Capital made this a natural win-win.”
The system was on the cusp of a healthcare emergency, so Sound had to act fast and designed an innovative model of care incorporating hospital medicine, telemedicine, new workflows, onboarding manuals, and virtually-hosted orientations in what was essentially a shell of a hospital. The care team included a day admitter, two telemedicine rounders, a nocturnist supplemented by telecrosscover at night, and bedside RNs. It was determined that using telemedicine was a perfect, cost-effective solution allowing for increased coverage without additional risk of exposure to COVID-19.

The plan was designed so that the telehospitalist would support and supplement onsite physicians with patient care, physician consultations, running rapid responses, and facilitating codes through synchronous video technology. In situations like the COVID-19 crisis, telemedicine can also be used to care for patients who are under isolation while in the hospital, which allows in-house clinicians to care for non-isolated patients without the risk of exposure to the pathogen.
“Despite many moving parts and a rapid implementation, our goal was, and continues to be, to do what’s right for every patient,” said Patel. “Our focus was to provide a unified approach to consistent, reliable care at the bedside and to maintain a human connection with families with regular meetings using Zoom and Facetime.”
“The feedback for this model of care has been positive and I think that’s because the team has been very collaborative, nimble and innovative,” said Dr. Greta Boynton, Chief Medical Officer. “We hope this robust utilization of telemedicine from start to finish can become the model of care going forward.”
