August 17, 2023
Emergency medicine is changing: Rising to the challenge
 How Americans seek acute unscheduled care is changing in ways that challenge traditional emergency department operations. As a national medical group with emergency medicine practices across the country, we‘re shifting our perspective and adapting to this change.
How Americans seek acute unscheduled care is changing in ways that challenge traditional emergency department operations. As a national medical group with emergency medicine practices across the country, we‘re shifting our perspective and adapting to this change.
What are the changes?
Volume is increasing — and, in some cases, exceeding pre-pandemic levels — but there are important differences in the types of patients seeking care. As the population ages and pediatric patients seek care at other venues, median patient age is increasing. Emergency departments (EDs) are seeing more medical illness and less trauma as life continues to become measurably safer, in large part due to fewer workplace accidents and improvements in automobile safety.
As well, substance abuse and mental health concerns continue to persist. Our EDs — and the health care system more broadly — struggle to serve patients dealing with these issues. Finally, acuity is greater than before. This is driven by the trends I’ve mentioned — and by the increasing availability of alternative sites of care for less complex patients. Those presenting to EDs are more likely than ever to require advanced imaging and admission to the hospital.
This overall increase in patient complexity has important impacts on throughput and the demands placed on the ancillary services supporting EDs.
What’s the impact on EDs?
The changes in the presenting patient population, combined with staffing shortages and lack of inpatient capacity, have led to high levels of dysfunction in many EDs.
“Exit blocks” exist in many hospitals — with many admitted patients held in ED beds. Length of stay has been rising as acuity rises, patient age increases, and many hospitals struggle with staffing and throughput for admitted patients. Nationally, the number of patients that leave the emergency department before completing their care has never been higher.
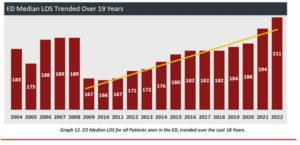
From 2022 EDBA Preliminary Report June 2023
‘No Surprises’ adds complexity
The No Surprises Act (NSA) and the 2023 documentation guideline changes have disrupted the economics of many emergency medicine practices. The NSA has provided needed protection for patients from aggressive billing practices, but it’s also disrupted insurance networks and delayed payment with a dysfunctional arbitration process.
Survey data from the Emergency Department Practice Management Association demonstrates that nearly 90 percent of claims submitted for arbitration have not been adjudicated. The NSA has been further complicated by multiple changes to rules and processes. Managing the emergency medicine revenue cycle has always required specialized expertise, but never more so than today.
How do we rise to these challenges?
Emergency medicine has always been a team-based endeavor, but a holistic approach to ED operations is more critical than ever, given the current climate. These are the things we see as fundamental to success.
- Strong on-site leadership. The biggest predictor of success at the local practice level is having a strong medical director who lives in the community they serve. And one of the benefits of a group like ours, with a national presence, is that if someone is facing a challenge, it’s likely we have a program and medical director elsewhere who has experienced that same problem – and successfully solved it. Our leadership is both community-based and collaborative, coast to coast.
- Strong recruitment. Building a great team is fundamental to success. We know that physicians recruit physicians, and advanced practice providers (APPs) recruit APPs. Physician-to-clinician internet groups are increasingly important as candidates search for positions. Our medical directors understand this changing landscape and create a great experience for applicants.
- Focus on well-being. We model our peer support program after one at Johns Hopkins, training physicians and APPs who are then available 24/7 to their peers for support around stress, malpractice claims, patient complaints, and any other issues of the moment in emergency medicine.
- Invest in development. We invest from the start in physicians who understand how to manage change, and can use data to guide effective decision-making.
- Documentation acumen. Partnering with an expert in the changing reimbursement landscape can make a huge difference in documenting correctly and setting up your practice and clinicians to be paid appropriately.
- Data and experience. Data outputs are helpful to a point; combining data analysis with on-the-ground expertise gets the best results. And while standardization can help improve generally, our focus is practicing medicine locally while sharing best practices across our emergency medicine programs.
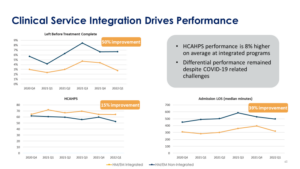
- Integration. Our integration with hospital medicine is critical to ensure we’re making optimal use of limited inpatient capacity. When we partner with hospitals across both service lines, we see objective improvement in both programs.
Where do we go from here?
Emergency medicine practices across the country are facing new challenges, but we’re excited about what the future holds. In following the approaches we’ve outlined, you’ll be better equipped to navigate this moment in emergency medicine.
For more on this subject, check out my webinar in partnership with Becker’s Healthcare.
