
Recently, I found myself in front of a small group of first-year medical students leading a discussion about a complex patient. Up until this session, the students had been hard at work learning to apply the tools of history taking, physical exam, and data collection to arrive at a diagnosis and “solve” the case. However, this would be their first encounter in which these tools would not yield a clear solution; I emphasized this point as I introduced the case.
“Doris” was elderly, lived alone, and had multiple complex medical issues. After suffering injuries related to a fall in her home, she admitted to the hospital. After ten days in the hospital, Doris was refusing most of the medications and treatments recommended by her care team. Steadfastly, she refused a short stay in a skilled nursing facility, though her physical therapist felt she was severely at risk for falls at home. Doris planned to return to her apartment and treat her edema, uncontrolled blood pressure, and uncontrolled blood sugars with the small pharmacy of herbs and supplements that she kept at her bedside.
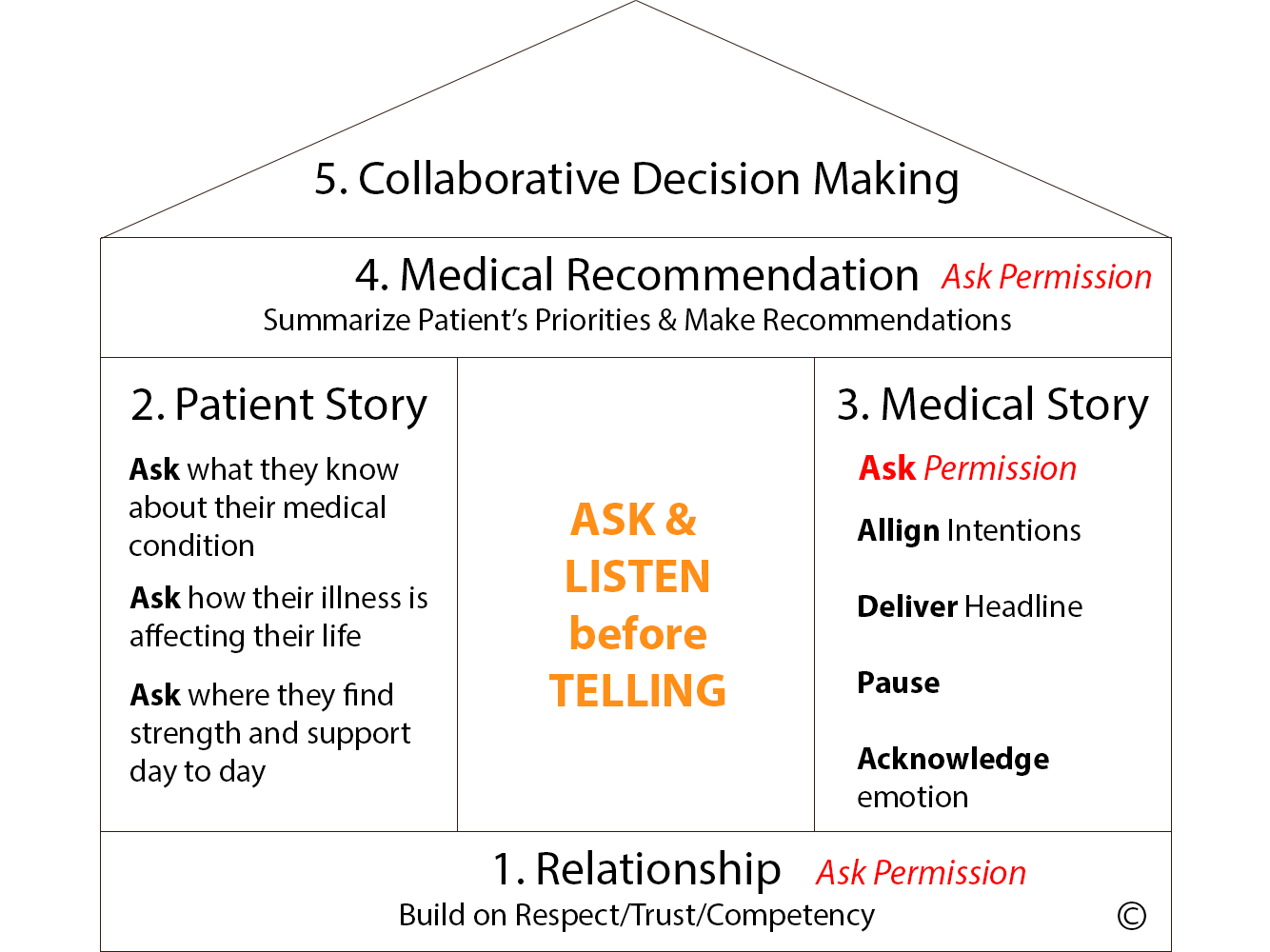
Although Doris is someone we encounter nearly every week, it was still enlightening to watch the students grapple with the situation, which led to a discussion on goals of care. “Did anyone ask Doris what she wanted?” asked a student. “Aha!” I thought. From there, I was able to help the students connect the dots with the goals of care and the “House Model” we use at Sound Physicians. The House Model outlines a procedure of specific steps to elicit a patient’s priorities in the setting of serious or advanced illness. The “house” refers to a visual framework of the five steps to use in navigating the goals of care conversation.
As we talked about the tools used to build the “house” and its components, I saw looks of confusion and frustration replaced by understanding and expressions of compassion. The familiarity of this transformation struck me; I had seen it many times with patients and families when I used the House Model to guide goals of care conversations.
In the students’ moment of understanding, the power of the house model was especially obvious; there was even a sense among the students that “the case was solved.” In my introductory remarks, I emphasized to the students that cases like Doris’ are rarely ever solved. Yet, towards the end of the session, I saw they arrived at a compassionate solution, one that preserved Doris’ right to self- determination and used the house model.
The next time that you find yourself at the bedside puzzling over a patient like Doris, scratching your head over a problem of disposition, communication, or adherence, ask yourself, “Is it time to pull out the tools and build the house?” If the answer is yes, get out your blueprints and get to work!
