Meeting Your Patient
Ms. Jones, an 82-year-old retiree presents for scheduled elective hip replacement surgery to alleviate the pain of her severe osteoarthritis. Along with a history of hypertension and mild cognitive impairment, her family has noticed her slowing down, losing weight, and feeling fatigued to the point where she needs assistance throughout the day. As the clinician overseeing her anesthetic care, why should you be concerned?
Diagnosing Frailty
Frailty is an age-related syndrome characterized by physiological decline, marked vulnerability, and reduced tolerance to medical or surgical stressors. The condition is cumulative, involving deficiencies throughout a patient’s various bodily systems and functions. Those at risk of frailty may be advanced in age, declining functionally, experiencing poverty, lacking nutrition, or living with medical or psychological issues contributing to their overall health.
While not all elderly individuals are considered frail, there is significant variability in this condition’s diagnostic criteria and classifications. When evaluating a patient for frailty from an anesthesia provider’s point of view, the main objective is to provide risk stratification and seek an opportunity for intervention to improve the patient’s procedural outcome, as well as their overall postoperative health.
Frailty Assessments in Surgery
Frailty assessments are crucial in identifying patients who are at higher risk of postoperative complications, mortality, and extended recovery times. Evaluations can occur well in advance of scheduled procedures or immediately prior to performing an anesthetic. Whether it’s in the preadmission testing clinic or the preoperative holding bay, taking frailty into consideration and addressing specific patient needs can reduce complications while improving the surgical experience for everyone involved.
Individualized Care Planning
Individualized care planning is crucial for patients with a condition as variable and cumulative as frailty. This requires a multidisciplinary team effort including coordination between anesthesia clinicians, surgeons, hospitalists, physical therapists, occupational therapists, nutritionists, social workers, and potentially hospice or palliative care consultants. Sound providers guide this process every day by synthesizing input from fellow clinicians, patients’ families, and patients themselves to construct the best course of action to meet an individual’s physical, emotional, and social needs.
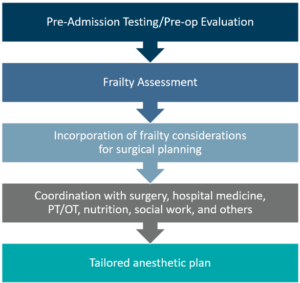
Each team leverages their respective expertise to construct a care plan that accounts for the patient’s needs and wishes while considering the impact on the healthcare system at large. For the anesthesia team, this includes accounting for the physiological differences of an older individual. Reviewing medications, optimizing baseline regimens, decreasing/delaying anesthetic doses, and limiting opioid use are just a few ways anesthesia providers avoid issues like postoperative delirium, prolonged sedation, or respiratory depression. In doing so, we play a vital role in reducing patients’ length of stay and supporting other teams after the postsurgical handoff.
The Cost of Frailty
Frailty increases healthcare costs not only on a routine basis but especially throughout the perioperative course. It is a significant cause of prolonged recovery times, postoperative falls, escalation of long-term care needs, and hospital readmissions- all of which require a greater utilization of resources including supplies and clinical support. Identifying and accounting for frailty early in the process can help mitigate these patients’ economic impact on the healthcare system.
So, how do we, as an engaged, multidisciplinary team, provide our 82-year-old patient, Ms. Jones, with the best possible care while avoiding high costs? With an early assessment, our team will recognize how her unique fragility has diminished her energy, ambulation, weight, and cognition- all of which help guide a tailored plan:
- Nutrition optimization and physical therapy to improve her strength and lessen her recovery time
- Postoperative support and a multimodal approach to manage her pain and help avoid injuries while limiting opioid-related side effects
- Family involvement will help ensure she has assistance with activities of daily living after discharge
Knowledge is Power
Frailty assessments are a crucial addition to an anesthesia team’s toolbox when it comes to providing cost-effective care. By identifying higher-risk patients, clinicians can anticipate complications and take appropriate measures to avoid them. Knowing your patients, taking every precaution to maximize their recovery, and conserving resources for all is the mark of an incredible clinical team.
Learn more about how our anesthesia teams enhance surgical outcomes with frailty assessments in this webinar.
