February 6, 2018
Proud, Grateful, and Inspired
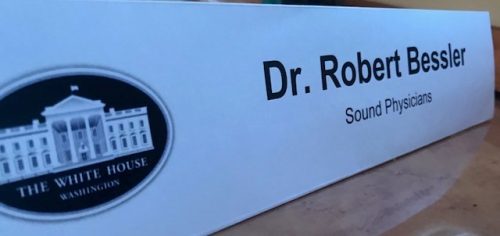 Recently, I had an experience that made me really proud. Proud to be an American, proud to be a physician, and proud to be leading an organization committed to driving better outcomes for patients. A few weeks ago, I received an email that contained an invitation to meet with members of the White House team to discuss electronic health record system interoperability. I honestly thought the email was spam. I even forwarded the email on to a colleague in D.C. with contacts in the West Wing to see if it was legitimate. Indeed, it was real. The invitation came from the Office of American Innovation to meet in the Roosevelt Room in the West Wing of the White House with the Administrator for the Centers for Medicare and Medicaid Services, Seema Verma, Jared Kushner, Senior Advisor to the President, Chris Liddell, Special Assistant to President on Strategic Initiatives, and Don Rucker, MD, Chief of the Office of Healthcare IT. I joined ten other healthcare executives to discuss the challenges of electronic health record (EHR) interoperability.
Recently, I had an experience that made me really proud. Proud to be an American, proud to be a physician, and proud to be leading an organization committed to driving better outcomes for patients. A few weeks ago, I received an email that contained an invitation to meet with members of the White House team to discuss electronic health record system interoperability. I honestly thought the email was spam. I even forwarded the email on to a colleague in D.C. with contacts in the West Wing to see if it was legitimate. Indeed, it was real. The invitation came from the Office of American Innovation to meet in the Roosevelt Room in the West Wing of the White House with the Administrator for the Centers for Medicare and Medicaid Services, Seema Verma, Jared Kushner, Senior Advisor to the President, Chris Liddell, Special Assistant to President on Strategic Initiatives, and Don Rucker, MD, Chief of the Office of Healthcare IT. I joined ten other healthcare executives to discuss the challenges of electronic health record (EHR) interoperability.
The desire to make a difference
I was struck by the intellectual curiosity of Kushner, Liddell, Verma, and Rucker and their desire to make a difference. An opening comment from Mr. Kushner resonated with me. In his government role and focusing on veteran’s issues, he learned it can take six months from when a soldier leaves the Department of Defense to have their chart transferred to the VA’s health system. With passion, he stated that the DOD can drop a missile on a pin anywhere in the world, so we certainly should be able to deliver healthcare information of the men and women who risk their lives each day much faster than we do today. This is an issue important to all Americans. The group addressed a few key questions:
- How important is EHR interoperability and why?
- What are the barriers to interoperability, and how might we overcome them together?
- Are there regulatory burdens we should examine to expedite the efforts?
- What approaches do you recommend to provide maximum benefits to the patient?
- What other important factors should we be considering?
The group agreed that access to good information is paramount. Most people don’t realize having bad information in healthcare kills between 220,000 and 400,000 patients per year (the third leading cause of death). If this was widely known, it would be considered an epidemic and perhaps get the same attention as the opioid crisis is getting today. During the meeting, I sat to the right of Chris Liddell and across the table from Administrator Verma. At one end of the table was Jared Kushner, and at the other end, Dr. Don Rucker. Spread amongst us were leaders of medical societies, healthcare systems, and a few national primary care physician groups.
Focusing on the acute episode of care
In my opening remarks, I spoke about how Sound is focused on the acute episode of care. This is important because more than 50% of healthcare spending in the United States occurs from the time a patient is admitted to the hospital through 90 days post-discharge. Currently, about 65% percent of this spending occurs after a patient leaves the hospital. If we are to improve quality/cost for all Americans, we must focus on these critical acute care episodes, and particularly on maintaining continuity of care as patients transition from the acute to the post-acute setting. In Sound’s many practices across the country, we have elevated this focus on transitions by participating in the Bundled Payment for Care Improvement Program (BPCI), an alternative reimbursement model sponsored by the Centers for Medicare and Medicaid Innovation (CMMI). BPCI gives providers a clear funding mechanism for investment in the people, processes, and technology required for great transitional care. Sound has embraced BPCI and is the the largest participant (health system or physician group) in the program. I am really proud to report that we reduced readmission rates by 20%, lowered skilled nursing home days by 5 days per patient, and reduced the cost of care more than 7% in the 90-day episode. Our efforts have resulted in resounding success, and we feel we are just scratching the surface of what’s possible. I expressed my appreciation to Administrator Verma for supporting the BPCI-Advanced program recently announced. CMMI took great care in rolling out the next version of BPCI, incorporating feedback provided by Sound Physicians and other healthcare organizations to make BPCI-Advanced even better. Despite our success in managing care bundles throughout the acute episode, we are challenged each day with the fragmentation of information. We have 17 years of experience managing inpatient and post-acute care, and our providers care for more than 1 million unique hospitalized patients annually. Patients are referred to our practice from more than 40,000 community providers across the country for inpatient care. Our workflow platform interfaces with referring providers, more than 300 hospitals, hundreds of nursing homes, and home health agencies in a vast variety of formats. This makes the issue of interoperability of paramount importance to Sound. I had the opportunity to opine on the subject of interoperability that my team helped me synthesize in advance of the meeting, focusing on three themes:
- Fragmentation. Interoperability is essential for optimal clinician performance, and thus for patient care quality – period. Optimal continuity of care cannot be achieved without interoperability of electronic health systems.The most serious quality and cost issue in U.S. healthcare is the fragmentation of care delivery. This issue cannot be addressed at scale without interoperability of EHR systems. Interoperability is also essential for efficiency. Billions are spent by the healthcare provider community on the replication and transfer of healthcare data between systems that are not interoperable. Billions more are spent due to lack of access to real-time, critical healthcare data, which results in an unnecessary and redundant utilization of services.
- Data Accessibility. Looking at system interoperability is the wrong paradigm – it is a goal that cannot be practically achieved. We need to look at data accessibility, which solves the problems created by systems that are not interoperable in a practical manner. We have experience with Health Information Exchanges (HIE) sponsored by some states and municipalities, which have created great benefits.However, there are two primary barriers to data accessibility. First, there are no requirements for either EHR vendors or providers to make critical clinical data accessible to qualified users. Second, making data accessible is costly and there is no reimbursement or financial incentive directly related to the goal of making data accessible.Data accessibility is like a public good – we all benefit, but no one party is in a position to pay for it. We can overcome these barriers by creating a compelling incentive (penalty, reward or both) for making an essential clinical dataset available for secure interchange with qualified users. “Qualified users” are healthcare providers who are engaged in the direct care of patients whose essential clinical data is to be shared. Providers and quality forums like NQF and NCQA can collaborate to determine the contents of the essential clinical dataset.
- Security. Additional requirements for data accessibility include patient consent to sharing data between providers, security of the data repositories housing this information, and the interfaces that access them.
While I focused on the essential clinical dataset, I suggested that immediately the government could take a stand on HL-7 interfaces and the newer FHIR standard. For non-IT readers, HL-7 is a standard templated format of how to send and receive mostly demographic data in a hospital. However, even these templated formats can create challenges. For example, an EHR system at a hospital may use the number 1 to identify male gender and the number 2 for females, where others may use other conventions. Conversely, a nursing home might use A or B to indicate gender.
Place patients at the center
While I know the current administration is trying to cut regulation and believes in a free market, a solution could easily be implemented to enforce standards for nomenclature that also benefits the greater good. Longer term, we could get to the essential clinical dataset recommended above. I made my point clear – LET’S PLACE PATIENTS AT THE CENTER, NOT THE ELECTRONIC HEALTH RECORD. I was impressed by the follow-up questions each participant asked of my peers and me. Mr. Kushner and Mr. Liddell responded favorably to my call to action and asked if there was anything else the government could do, and I responded, yes! The government could force the implementation of a unique patient identifier for every patient in the country, instead of the crazy approach of matching patients up with different identification numbers in different settings. The current practice creates an incredible administrative burden and leads to countless errors. One of my favorite lines from Administrator Verma was “patients over paperwork.” Who can argue with that? As the meeting wrapped up, I was inspired by the desire of these former private sector individuals who are trying to make a meaningful difference for all Americans, centered on the idea of bringing people together from the “real world” to produce ideas and map out the path forward. It gave me confidence that these issues could be tackled. Bringing people together from all parts of the healthcare economy combined with the august setting of the meeting gave me the powerful understanding that the White House really is “America’s House.” I can’t wait to see where these discussions lead, and I look forward to returning soon. As we exited the West Wing through the patio, I felt deep gratitude for the opportunity to lead a dedicated team of professionals who are working tirelessly to improve quality and lower the cost of care for patients in each community we serve.
