January 9, 2024
Medicare Advisor: Timely and appropriate conversion from observation to inpatient
By Rob Zipper, MD, MMM, SFHM, Chief Medical Officer, Physician Advisory and Health Policy
Medicare Advisor is Sound Physicians’ solution to a nearly ubiquitous problem: patients are often discharged under observation services when they would have been appropriate for inpatient. At some of our partner hospitals, despite many having excellent case management programs, more than 50 percent of traditional Medicare observation discharges were patients that were hospitalized spanning at least two midnights.
This results in lost revenue for hospitals, and typically leads to greater patient out-of-pocket expenses.
What happens in typical case management programs is that observation patients are placed in a queue and reviewed once per day. This time frame isn’t fast or frequent enough to identify patients appropriate for inpatient and get the inpatient order written prior to a discharge order being written, after which it is too late. For example, if case management reviews a case (after one midnight) at 10 a.m. and it isn’t clear that the patient will qualify for inpatient status at that point in time, observation will likely be recommended. If the attending decides that the patient has medical necessity for a second midnight, but the patient is discharged the following day prior to another case management review, that patient that has met the criteria of the Two-Midnight rule might well be discharged under observation. Another common scenario is that case management processes use MCG or InterQual for status determination on Medicare fee-for-service (FFS) patients, despite these guidelines lacking any weight for traditional Medicare patients.
Medicare Advisor is focused on nearly real-time monitoring and review of these cases. By using lists of Sound Hospital Medicine patients from our proprietary charge-capture platform, SoundConnect, we have nurses monitor the charts of patients in observation and promptly have a Sound Physician Advisor — one of our experts in clinical documentation and compliant status determinations — review the clinical documentation. If inpatient status is supported, they then securely contact the hospitalist to discuss the inpatient recommendation, and do some teaching as needed. The entire process is coupled with robust education for hospitalists on the details of status assignment, prior to implementation.
In 2023, we focused solely on Medicare FFS patients, and we’ll share typical results below. But as of now (as clarified in the 2024 MA Final Rule CMS-4201-F), Medicare Advantage (MA) payers must also follow the provisions of the Two Midnight rule, the Case-by-Case Exception, and the Inpatient-Only list. While it’s true that MA payers can change status after discharge, typically MA cases are not reviewed by case management once they are discharged as observation, or if the case fails to meet inpatient criteria by MCG or InterQual. By the Two-Midnight Rule, as long as medical necessity is present, many (if not all) of these cases would be appropriate for inpatient status. CMS has written that while MA payers can use clinical criteria, such criteria cannot be the final word when it comes to status assignment. For patients that meet medical necessity requirements for a stay exceeding two midnights, MA plans are obligated to pay inpatient DRGs. While there is still a lot of uncertainty as to how MA plans will respond to the rule clarifications, we’re excited to expand our Medicare Advisor program to include Medicare Advantage patients and further support our partner hospitals.
In terms of results so far, we’ve seen several significant changes, including:
- Recovering previously lost revenue (Medicare FFS average per hospital is $700K annually)
- Freeing up time lost to case management queries.
- Improved regulatory compliance and decreased audit risk.
- A 36 percent average drop in Medicare FFS observation discharges longer than two midnights, which results in length-of-stay improvement for both inpatients and patients under observation.
Our program seamlessly integrates with your Sound Hospital Medicine program through our proprietary patient tracking and billing platform, SoundConnect. No additional technology is required.
Medicare Advisor: One Sound Hospital’s Results
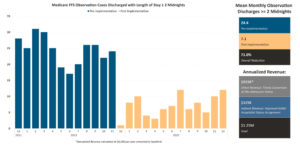
The results have been significant with reduction in observation discharges spanning at least two midnights. The overall reduction (at all Sound Partners) is 63.4 percent with long observation discharges, and 71 percent in this example. Revenue improvement is captured from timely Physician Advisor case review and conversion of observation to inpatient, and from improved initial hospitalist status assignment as a result of educational efforts. For this facility, annualized revenue is $1.25M from the Medicare Advisor Program.
