September 16, 2021
CDI Week and Documenting COVID-19

Clinical Documentation Week coupled with the recent COVID resurge across the country is another poignant opportunity to remember the importance of complete, specific, and appropriate documentation to avoid inappropriate COVID denials. Just as this tiny virus caused huge impacts, small changes in documentation have caused significant losses of vitally important revenue to our healthcare systems. With uncertainty regarding fiscal year reimbursements, elective surgeries volumes, and staffing, it is more important than ever for hospitals to get reimbursed at the appropriate level for the care of very sick patients, including patients with COVID-19.
Of course, first and foremost, we want to provide the interventions and treatment needed to restore our patients’ health and protect our communities. But, we also need to take care of the financial health of our hospitals. Complete, specific, and proper documentation will not only help the healthcare system’s revenue cycle but will also help prevent retrospective audits and improve quality metrics for individual clinicians. How do we address this challenge? We must provide a higher level of specificity and clarity for cases where multiple conditions are contributing to making a patient very sick. The health of our hospitals depends upon us making this effort.
Documentation Tips for COVID-19
Coding for Risk Adjustment:
- Diagnose/document using coding-based language as much as possible
- Make sure the diagnosis(s) is in the chart at least once
- Document to the greatest level of specificity. Clinically support the documented diagnoses with lab, radiology, or other test results to fully defend each one
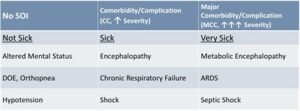
- Secondary Diagnoses: bucket into one of 3 groups – Not sick, sick, and very sick.
CDI Tips for COVID-19
Be specific with the following:
- Pneumonia – type, viral, bacterial (Gram Neg, MRSA, etc.), Aspiration?
- Respiratory Failure – Acute, Chronic, Acute on Chronic?
- Sepsis – Septic shock, underlying infection, organism?
- Renal Failure – AKI, ATN, CKD, and stage?
- Type 2 MI – Demand Ischemia, underlying cause?
- Coagulopathy- is it associated?
- DIC- is there a relation?
- Thrombotic microangiopathy- link if appropriate
- Metabolic Encephalopathy- expand on the status of the patient’s mentation related to the effects of COVID-19
The New COVID-19 ICD-10-CM Code
- Applies to all patient types.
- The intent is to code for only confirmed cases of COVID-19.
- Provider’s diagnostic statement or a positive COVID-19 test result, assign code U07.1.
- The link between a positive test result and acute respiratory condition is not required.
- If COVID-19 test results are positive after discharge (far less likely than it was early in the pandemic when we had limited testing capabilities and longer turnaround times), Code U07.1 may be used.
- Assigning U07.1 as the principal diagnosis depends on the circumstances of admission.
- Other COVID-19 specific codes:
- Multisystem inflammatory Syndrome from COVID-19 (M35.81) CC
- Pneumonia due to COVID-19 (J12.82) MCC
- Other specified systemic involvement of connective tissue (M35.89) CC
It’s essential to keep in mind that the principal or secondary diagnosis of COVID-19 is based on the physician’s clinical judgment of how sick the patient is, notwithstanding a positive or negative test. Please remember that specificity is critical, not only for COVID-19 but for all documentation in the chart so that appropriate diagnoses, DRGs, and quality metrics to be assigned. Changing a few words can have an enormous impact on accurately portraying the severity of illness and the associated medical necessity issues.
Amid all of the confusion and uncertainty this pandemic has caused, this steadfast principle remains clear: the only defense against inappropriate COVID-19 denials is complete, specific, and appropriate documentation. Providers who paint a picture with their words significantly reduce the risk of being denied full reimbursement for treating these incredibly sick patients.
