OVERVIEW
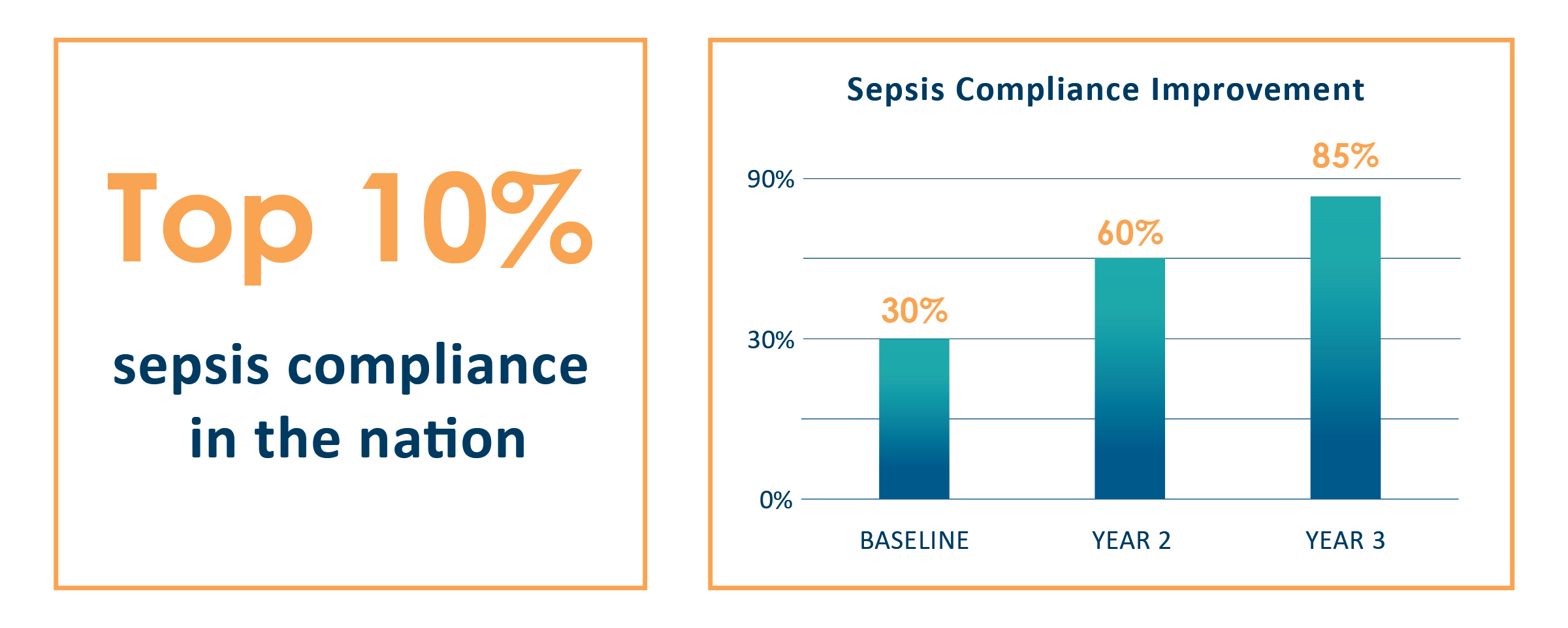
At a small Northwest hospital, the emergency medicine team was struggling to implement protocols that would satisfy the sepsis bundle, first introduced in 2015 by the Centers for Medicare and Medicaid (CMS), while also bringing meaningful care to patients who were dealing with the condition. Compliance hovered around 30 percent, and while the hospital had a sepsis committee, it required more involvement and a clear vision for seamless alignment of care throughout the hospital.
Sound’s medical director saw an opportunity to improve compliance by making a compelling case with clinicians and administrators around the importance of catching and treating sepsis in the emergency department. Through continued engagement and education, the team saw truly consequential change in the first year, with compliance at 65 percent. Within two years, the hospital’s compliance is now at 85 percent — and in the top 10 percent in the nation.
OPPORTUNITY
With a complicated algorithm and demanding documentation requirements, the sepsis initiative felt more an impediment to clinicians’ workflows than a support to patients. The medical director saw an opportunity to appeal to clinicians about the threat and fatality of sepsis. Frank conversations across the team acknowledged what they were feeling: Yes, it was a complicated process and difficult to navigate in a busy shift, but ultimately the right thing to do for the patient.
When clinicians could appreciate the gravity of sepsis along with the acknowledgment that there was room for improvement, the medical director found buy-in from his emergency medicine team, and from hospital administrators, nurses, phlebotomists, housekeeping staff — everyone who cared for and about that patient while in the emergency department (ED).
To meet the sepsis bundle requirements, the team needed to get much tighter on timing of procedures, including lab draws, imaging, and IV fluids. They would need to revamp their systems and processes in such a way that everyone was aligned and operating from the same playbook.
WORKING TOWARDS COMPLIANCE
TRANSFORMATIVE CHANGE
With a cohesive approach in place, the medical director took a number of steps to shore up compliance:
- Feedback and education. He identified places where the team wasn’t compliant already — including drawing labs in the appropriate window of time and administering the recommended dose of fluids — and provided immediate feedback on the appropriate course-correction in an educational way.
- Labs. He asked physicians to embrace the idea of nurses ordering labs that physicians normally would. This has allowed patients to be diagnosed and treated sooner.
- ED blood draws. To assist in expediting labs, nurses set up a curtained lab station in the waiting room. For patients who presented with sepsis symptoms, the team was able to fast-track a blood draw, which patients greatly appreciated.
- Printed guidelines. The team created quick-reference cards that clinicians and staff carried with them or had on hand in the places they would be managing and treating sepsis patients. These equipped the team during a busy shift with guidance on the signs and symptoms of sepsis.

With these systems and processes in place, the team was able to operate consistently and know what to do and when, and how to document it in the ways that would yield greater compliance rates. The emphasis was not only on following the recommended protocols but also on documenting when they were unable to treat with the recommended protocols and why, and how they were mitigating those protocols.
Ultimately, compliance became a point of pride, rather than a point of contention, for the hospital and the clinicians alike.
KEY RESULTS